Mathematical equations that reproduce the most fundamental aspects of living processes and cells are being sought by scientists around the world who hope to weave them together to simulate tissues, organs and even create ‘virtual humans’.
To complement the Science Museum’s plans for the £24m Medicine Galleries (due to be completed in 2019) to showcase the extraordinary collection of Henry Wellcome, a glimpse of the future of medicine was presented to a packed Lates audience last month by four leading proponents of the €5 million CompBioMed Centre of Excellence in Computational Biomedicine.

Just as a weather forecast relies on a mathematical model of the Earth’s atmosphere, run in a supercomputer using data from meteorological stations, satellites and so on, the team hope to glean mathematical models of the body with an individual person’s data, from their DNA code to body scans, to forecast their health.
After the IMAX premiere of a film about the potential of the virtual human project by Fernando Cucchietti and Guillermo Marin of the Barcelona Supercomputer Centre, there were presentations, a discussion and Q&A which you can listen to here.
Although we are still years away from virtual humans, huge progress has been made in key parts of the project; Prof Peter Coveney of University College London, who leads the CompBioMed consortium, discussed his work to simulate how drugs that treat diseases such as cancer and Aids work in the body.
Rather than the current approach taken by the pharmaceutical industry, of producing ‘one size fits all drugs’ that may not work well in some people, or cause side effects in others, Prof Coveney is studying how to select the right drug to treat an individual patient by simulating the structure and motion of a target protein in their body that potential drug molecules act on.
When it comes to preventing serious side effects, Prof Blanca Rodriguez of the University of Oxford told the audience how her work on the virtual heart can, for example, help understand how antihistamines can cause sudden cardiac death.
She said that in addition to tests on animals, patient cells and patients, her team hopes these simulations will one day help warn of potential problems with prescribed drugs. Though “challenging”, they are already working with the industry on medicine safety, she said.
So far, her team has shown computer simulations based on virtual cells provide better accuracy than animal experiments in predicting adverse side effects on the rhythm of the heart.
Prof Marco Viceconti of Sheffield University, a key player in the Virtual Physiological Human initiative, talked about the challenges in simulating the complexity of the human body which is made up of 20,000 genes, 90,000 proteins, myriad protein combinations, 40 trillion cells along with three times more microbial passenger and parasite cells – “What amazing complexity.”
He demonstrated how his team has simulated the muscles and skeleton of a virtual human by animating one to the sound of La Macerena:
“We can predict the forces expressed by every single muscle in this young man who is dancing, the forces that can fracture the hip of an elderly lady affected by osteoporosis, or the forces transmitted in the pelvic floor of a woman in childbirth.”
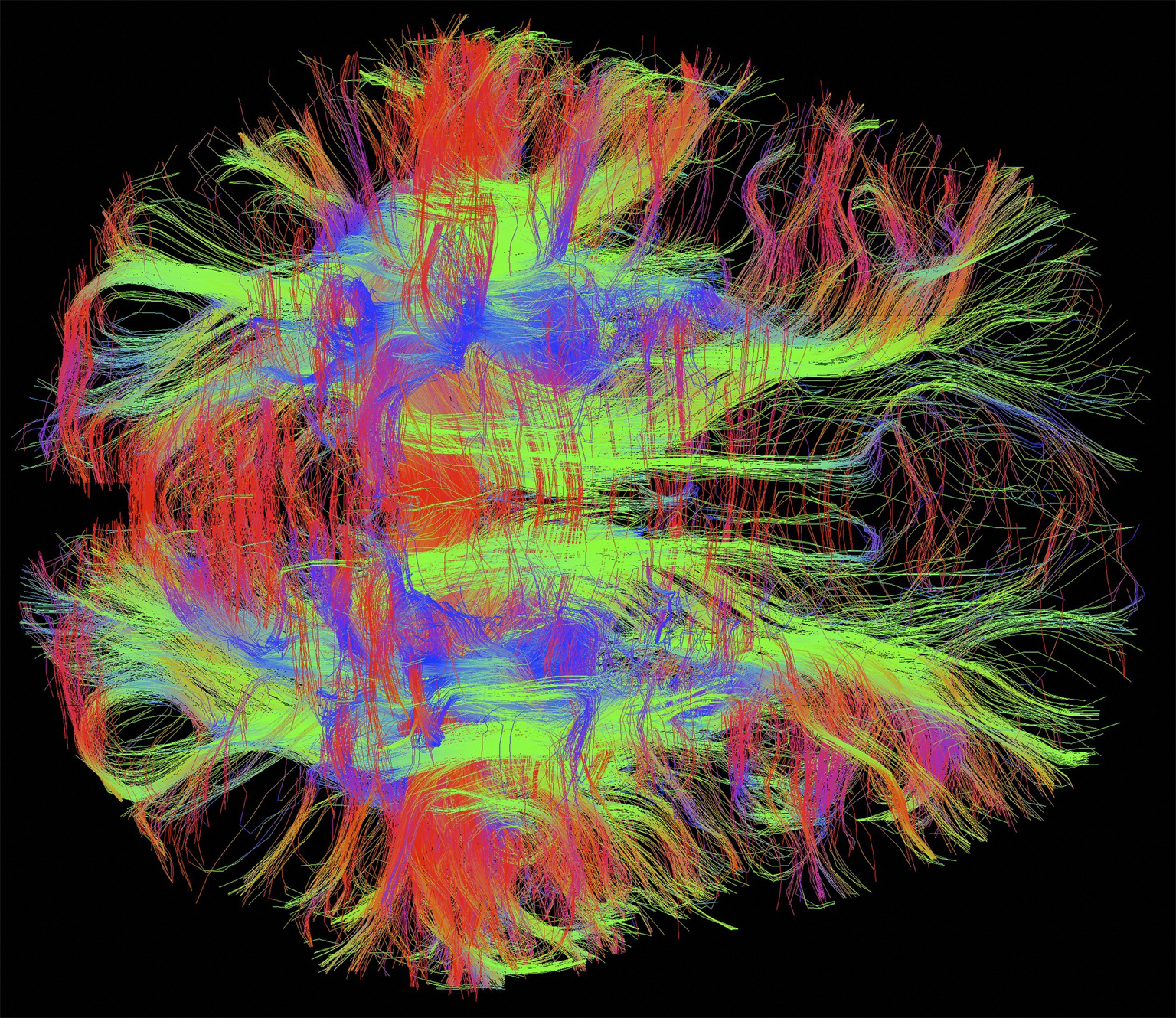
Prof Alfons Hoekstra of the University of Amsterdam discussed the efforts of his team to construct virtual arteries. “Blood is beautiful,” he announced to the audience. “Look at this movie – you can see the red blood cells flowing through this artery.”
Using computer models, we can study the swelling of an artery in the brain, called an aneurism, and predict if a patient is at risk of a rupture, or to simulate the movement of blood clots through the body:
“We want to help doctors select the best treatment options. With the help of their virtual human, it should be possible to customise the right treatment for any given patient. We are working very hard …to achieve these goals.”
Prof Coveney also believes that the kind of theory being developed for the Virtual Human Project will help reveal which kinds of patient data are the most useful and how best to interpret them: spurious correlations are a familiar problem to those who use machine learning to find promising drugs and he believes that big data require theory and understanding to interpret properly.
The number and scale of medical data sets, though growing all the time, still afford us an impoverished view of the complexity of the human body. Bodies are dynamic and ever-changing, while traditional data sets often only give snapshots at a specific moment.
Another issue is that data are not always reliable (‘Why most published research findings are false’ as famously reported by John Ioannidis of Stanford University in PLOS Medicine).
Prof Coveney hopes that one day a doctor will be able to study the way diet and treatments work via your digital doppelgänger before they try it out on you. With the birth of the first virtual humans, we will have the beginning of truly personalised medicine.