The short life of Tsarevich Alexei, explored in The Last Tsar: Blood and Revolution exhibition, was blighted by the bleeding disorder haemophilia. Dr Matthew Lumley, Rare Disease Medical Director, Pfizer UK, explains how the future is much brighter for today’s sufferers.
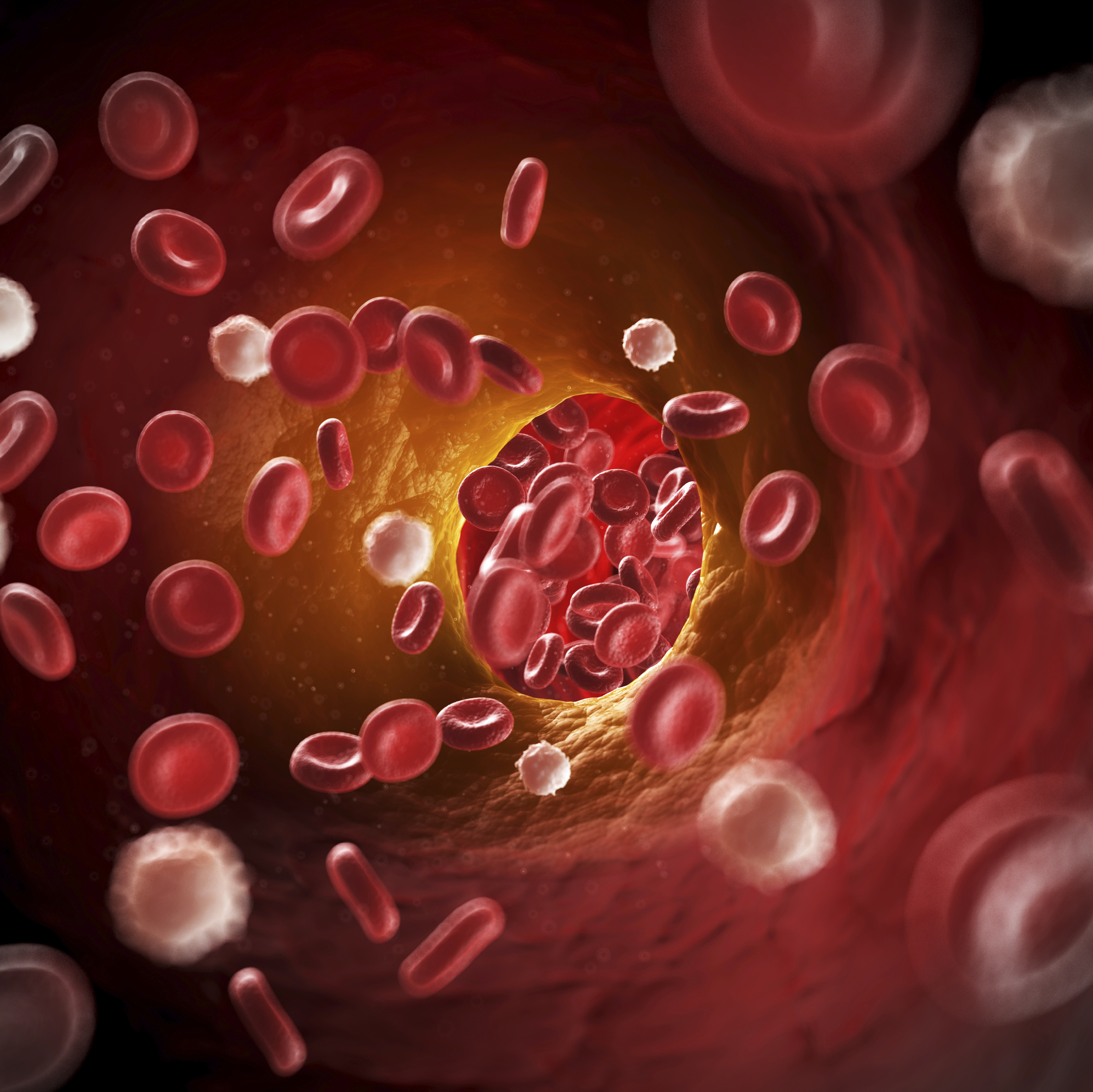
If you cut yourself, you stop bleeding because proteins in blood, known as clotting factors, combine with blood cells called platelets, making the blood sticky and causing it to clot. People with haemophilia are either missing an essential clotting factor or are unable to produce enough to make their blood clot. The severity of haemophilia is determined by the type of clotting factor that is deficient and also how much of the clotting factor is made. In severe haemophilia, a person may bleed once or twice a week, and often for no apparent reason. About 10,000 people in the UKhave haemophilia.
The Royal Disease
The haemophilias are typically caused by a single gene mutation on the X chromosome, which means the condition largely affects men and boys. Boys like Tsarevich Alexei, born in 1904, who inherited haemophilia B, via his great grandmother Queen Victoria.
Until the advent of treatment, most people with severe haemophilia died in childhood or in early adulthood. Even in the 1960s, when treatments were available, it was still not possible to successfully prevent major bleeds. This inability to adequately manage haemophiliac bleeding made the condition very debilitating.

The Modern Era
By the 1970s, it was possible to make enough human-derived clotting factor to enable people to treat themselves at home. The change was revolutionary: haemophilia centres were able to change their focus from emergency care to developing care programmes aimed at improving the quality of life for people living with haemophilia.
But in the 1980s, it was discovered that much of the human-derived clotting factor had come from blood donations contaminated with blood-borne diseases, HIV and hepatitis viruses; thousands of people were infected and thousands subsequently died. Improved screening and new methods to deactivate viruses improved the safety of donated blood, but concern continued about the safety of human derived products.
Medical advances and clinical research in the 1980s and 1990s led to the development of man-made, ‘recombinant’ clotting factor that allowed for the industrial production of clotting factor and eliminated the risk of blood-borne infection. The availability of recombinant clotting factor has meant that people with haemophilia now have a normal life span.

Into the Future
Today, haemophilia is a treatable rare disease; however, frequent infusions of clotting factor are time consuming and have a considerable negative impact on the quality of life of patients with haemophilia.
Treatment of haemophilia continues to evolve. Novel treatments that activate clotting rather than replace missing clotting factors have already arrived. Treatments in development include those that suppress the body’s natural ability to prevent clotting. One technology that excites people is gene therapy, which works by introducing corrected copies of missing or defective genes. In the case of haemophilia, the goal is to get the body to make the correct version of the missing clotting factor. If this could be achieved then, for some patients, it might be possible for haemophilia to be managed with a single treatment, reducing or even eliminating the need for treatment with replacement factors, thus greatly reducing the burden of this disease on patients and their loved ones.
This blog was written alongside our recent exhibition The Last Tsar: Blood and Revolution, exploring the life and death of Tsar Nicholas II and his family and the forensic investigation into their murder. Discover more about the science behind one of the greatest mysteries of the 20th century in this series of blog posts.